- Home
- Prelims
- Mains
- Current Affairs
- Study Materials
- Test Series
 EDITORIALS & ARTICLES
EDITORIALS & ARTICLES
Understand the virulence of your Viruses
Predominantly, viruses have a reputation for being the cause of contagion. Widespread events of disease and death have no doubt bolstered such a reputation.
Every new virus that surfaces puts the scientific fraternity on red alert, for viruses have a notorious reputation for posing unprecedented challenges. Some (such as Ebola) are lethal with a high mortality rate, whereas others (like the coronavirus) transmit rapidly.
12 deadly viruses
| Marburg virus Scientists identified Marburg virus in 1967, when small outbreaks occurred among lab workers in Germany who were exposed to infected monkeys imported from Uganda. Marburg virus is similar to Ebola in that both can cause hemorrhagic fever, meaning that infected people develop high fevers and bleeding throughout the body that can lead to shock, organ failure and death. The mortality rate in the first outbreak was 25%, but it was more than 80% in the 1998-2000 outbreak in the Democratic Republic of Congo, as well as in the 2005 outbreak in Angola, according to the World Health Organization (WHO). |
| Ebola virus The first known Ebola outbreaks in humans struck simultaneously in the Republic of the Sudan and the Democratic Republic of Congo in 1976. Ebola is spread through contact with blood or other body fluids, or tissue from infected people or animals. The known strains vary dramatically in their deadliness, Elke Muhlberger, an Ebola virus expert and associate professor of microbiology at Boston University, told Live Science. One strain, Ebola Reston, doesn't even make people sick. But for the Bundibugyo strain, the fatality rate is up to 50%, and it is up to 71% for the Sudan strain, according to WHO. The outbreak underway in West Africa began in early 2014, and is the largest and most complex outbreak of the disease to date, according to WHO. |
| Rabies Although rabies vaccines for pets, which were introduced in the 1920s, have helped make the disease exceedingly rare in the developed world, this condition remains a serious problem in India and parts of Africa. "It destroys the brain, it's a really, really bad disease". "We have a vaccine against rabies, and we have antibodies that work against rabies, so if someone gets bitten by a rabid animal we can treat this person". However, "if you don't get treatment, there's a 100% possibility you will die. " |
HIV In the modern world, the deadliest virus of all may be HIV. "It is still the one that is the biggest killer". An estimated 32 million people have died from HIV since the disease was rst recognized in the early 1980s. "The infectious disease that takes the biggest toll on mankind right now is HIV". Powerful antiviral drugs have made it possible for people to live for years with HIV. But the disease continues to devastate many lowand middle-income countries, where 95% of new HIV infections occur. Nearly 1 in every 25 adults within the WHO African region is HIVpositive, accounting for more than two-thirds of the people living with HIV worldwide. 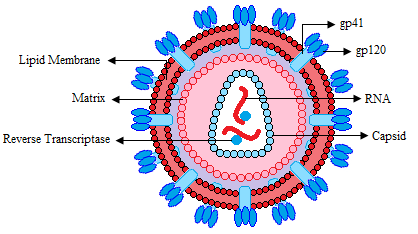 |
| Small pox In 1980, the World Health Assembly declared the world free of smallpox. But before that, humans battled smallpox for thousands of years, and the disease killed about 1 in 3 of those it infected. It left survivors with deep, permanent scars and, often, blindness. Mortality rates were far higher in populations outside of Europe, where people had little contact with the virus before visitors brought it to their regions. For example, historians estimate 90% of the native population of the Americas died from smallpox introduced by European explorers. In the 20th century alone, smallpox killed 300 million people. |
| Hanta Virus Hantavirus pulmonary syndrome (HPS) gained wide attention in the U.S. in 1993, when a healthy, young Navajo man and his FIancée living in the Four Corners area of the United States died within days of developing shortness of breath. A few months later, health authorities isolated hantavirus from a deer mouse living in the home of one of the infected people. The virus is not transmitted from one person to another, rather, people contract the disease from exposure to the droppings of infected mice. Previously, a different hantavirus caused an outbreak in the early 1950s, during the Korean War. |
| Influenza During a typical flu season, up to 500,000 people worldwide will die from the illness, according to WHO. But occasionally, when a new flu strain emerges, a pandemic results with a faster spread of disease and, often, higher mortality rates. The most deadly flu pandemic, sometimes called the Spanish flu, began in 1918 and sickened up to 40% of the world's population, killing an estimated 50 million people. |
| Dengue Dengue virus appeared in the 1950s in the Philippines and Thailand, and has since spread throughout the tropical and subtropical regions of the globe. Up to 40% of the world's population now lives in areas where dengue is endemic, and the disease — with the mosquitoes that carry it — is likely to spread farther as the world warms. Dengue sickens 50 to 100 million people a year, according to WHO. Although the mortality rate for dengue fever is lower than some other viruses, at 2.5%, the virus can cause an Ebola-like disease called dengue hemorrhagic fever, and that condition has a mortality rate of 20% if left untreated. |
| Rota Virus Two vaccines are now available to protect children from rotavirus, the leading cause of severe diaorrheal illness among babies and young children. The virus can spread rapidly, through what researchers call the fecal-oral route (meaning that small particles of feces end up being consumed). Although children in the developed world rarely die from rotavirus infection, the disease is a killer in the developing world, where rehydration treatments are not widely available. The WHO estimates that worldwide, 453,000 children younger than age 5 died from rotavirus infection in 2008. But countries that have introduced the vaccine have reported sharp declines in rotavirus hospitalizations and deaths. |
| SARS-COV The virus that causes severe acute respiratory syndrome, or SARS, first appeared in 2002 in the Guangdong province of southern China, according to the WHO. The virus likely emerged in bats, initially, then hopped into nocturnal mammals called civets before finally infecting humans. After triggering an outbreak in China, SARS spread to 26 countries around the world, infecting more than 8000 people and killing more than 770 over the course of two years. The disease causes fever, chills and body aches, and often progresses to pneumonia, a severe condition in which the lungs become infected and ill with pus. SARS has an estimated mortality rate of 9.6%, and as of yet, has no approved treatment or vaccine. However, no new cases of SARS have been reported since the early 2000s, according to the CDC. |
| SARS-COV 2 SARS-CoV-2 belongs to the same large family of viruses as SARS-CoV, known as coronaviruses, and was first identified in December 2019 in the Chinese city of Wuhan. The virus likely originated in bats, like SARS-CoV, and passed through an intermediate animal before infecting people. Since its appearance, the virus has infected tens of thousands of people in China and thousands of others worldwide. The ongoing outbreak prompted an extensive quarantine of Wuhan and nearby cities, restrictions on travel to and from affected countries and a worldwide effort to develop diagnostics, treatments and vaccines. The disease caused by SARS-CoV-2, called COVID-19, has an estimated mortality rate of about 2.3%. People who are older or have underlying health conditions seem to be most at risk of having severe disease or complications. Common symptoms include fever, dry cough and shortness of breath, and the disease can progress to pneumonia in severe cases. |
| MERS COV The virus that causes Middle East respiratory syndrome, or MERS, sparked an outbreak in Saudi Arabia in 2012 and another in South Korea in 2015. The MERS virus belongs to the same family of viruses as SARS-CoV and SARS-CoV-2, and likely originated in bats, as well. The disease infected camels before passing into humans and triggers fever, coughing and shortness of breath in infected people. MERS often progresses to severe pneumonia and has an estimated mortality rate between 30% and 40%, making it the most lethal of the known coronaviruses that jumped from animals to people. As with SARS-CoV and SARS-CoV-2, MERS has no approved treatments or vaccine. |
It is barely a century ago that we detected viruses, although they have been ravaging humanity for ages. It was only in 1901 that James Caroll and Walter Reed established that a virus was causing deadly yellow fever. Although they did not see the virus per se, they proved that the unknown, yet filterable pathogen, was smaller than the bacteria.
Viruses remained elusive to the eye until the advent of the electron microscope in the 1930s. It took another fifty years to see their structural details. Today, technology advancements provide us with greater clarity of their diversity. However, several aspects of their molecular functioning still remain to be understood.
Viruses are a class apart, neither living nor non-living entities, nor belonging to bacteria, plants or animals. Though they contain the primary life-juice – nucleic acid, they need a living cell to multiply, making them parasites. Viruses infect plants, animals and even bacteria, usurping the host cell machinery to replicate rapidly.

They are only a fraction of the 1400 or more species of pathogens that infect humans, and 250 known species exist. Studies indicate that in the past few decades, a majority of newly discovered infections have been due to viruses as each year three to four new species add to the list. There is yet a fair amount of unknown species.
Characteristics of Viruses:
All the viruses are minute and simplest organisms which can be observed only by the use of electron microscope.
The diameter of viruses ranges from about 20-30 mm on average. They are 50 times smaller than bacteria.
They are metabolically inactive outside the host cell because they do not have enzyme systems and proteins synthesis machinery. Thus, they are obligatory intracellular pathogens or parasite.
They are composed of nucleic acid either DNA or RNA or both and protein. The protein that surrounds the nucleic acid is called protein coat, the capsid.
Viruses do not have cellular structure i.e. they lack a true nucleus, cytoplasm and cytoplasmic organelles like mitochondria, Golgi complex etc.
During reproduction, the virus particle disorganized into molecular constituents inside the host cell. This phase is called eclipse phase.
They show respond to chemicals, heat, and temperature. Outside the host cell, they can be crystallized and behaves like the chemicals. They cannot show the independent mode of life. They are highly specific to their host.
Viruses cannot reproduce by fission or conjugation. They undergo mutation like living organisms.
Living Characters of Viruses
Viruses can grow and reproduce within the host cell.
The ultrastructure of most viruses shows similar morphological structure to bacteria like cocci. They undergo mutation like living organisms.
They have their own genetic material in the form of RNA, DNA or both.
They show intracellular parasitism and can be transmitted from the diseased host to healthy ones.
They are infective and capable of spreading diseases.
They respond to light, chemicals, and temperature.
Non-living character of viruses
They lack a complete cellular structure.
They lack enzyme system and do not have metabolic activity of their own.
Viruses do not respire. Some viruses can be crystallized and stored in bottles like chemicals.
They can be precipitated by a number of a chemical substance.
They depend upon living host for their existence.
They are with high specific gravity.
Viruses are nucleoprotein entities of high molecular weight and have the power of multiplication.
Viruses are self-assembled nanoparticles of a core of genetic material (either RNA or DNA, but not both), lipids, and proteins to cover the centre and invade host cells. Once inside a living cell, they hijack the manufacturing unit – ribosomes, using it to produce the viral protein patterns. At the molecular level, the ribosomes know how to follow instructions without the ability to differentiate the source. Another cell component – Golgi complex does the packaging. Soon, the cell detects the runaway production, shuts down by self-destruction to prevent further damage. The cell wall bursts open to get rid of the viral particles. However, this works to the virus’ advantage as they get released in the vicinity, invading more cells.
Each viral strain uses different tactics to invade cells. Gaining insights into the molecular changes that occur is active, ongoing research. One such effort on the new coronavirus, a team of researchers at IIT Kanpur is attempting to view the structural transformations in real-time mode. Using highly advanced imaging instruments, they hope to see how the virus fights our immune cells, docks with the human cell and opens a pore in the cell membrane to transfer its genetic material. Their study may offer clues to develop a vaccine for Covid-19.
What makes viruses so dreaded is their mutations. The RNA-type viruses (such as the new coronavirus) tend to mutate more than the DNA type because their genetic material lacks a supervising code. Unsupervised production leads to mistakes, which result in different protein structures from the original copy. The changes dramatically influence the type of cells to invade.
Viruses are positioned at the lowest rung of the evolutionary ladder and hence under the constant pressure of survival. So, the mutated virus has a primary motto to look for a matching pattern in a living cell, latch on, propagate and thrive.
Experts caution that in the past few decades, species crossover of viruses is on the rise due to increased human-animal interaction. Almost 80% of the known viruses are found to perpetuate in animals — farm as well as wild. As we share several molecular commonalities with animals, we are highly susceptible to viral mutations that cross over.
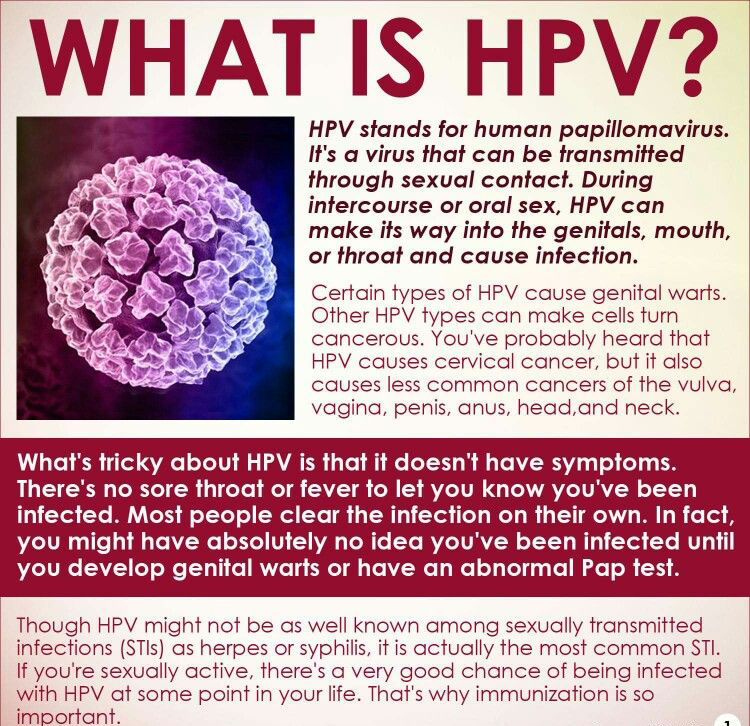
The Human Papilloma Virus vaccine has been making the headlines in the recent months. Who make the ideal candidates for receiving this vaccine and what are its benefits?. (UPSC 2012)
Retrovirus
A retrovirus is an RNA virus that is duplicated in a host cell using the reverse transcriptase enzyme to produce DNA from its RNA genome. The DNA is then incorporated into the host’s genome by an integrase enzyme. The virus thereafter replicates as part of the host cell’s DNA. Retroviruses are enveloped viruses that belong to the viral family Retroviridae. A special variant of retroviruses are endogenous retroviruses, which are integrated into the genome of the host and inherited across generations. Endogenous retroviruses are a type of transposon.
The virus itself stores its nucleic acid in the form of an mRNA genome and serves as a means of delivering that genome into cells it targets as an obligate parasite (a parasite that cannot live without its host). That process of delivering the genome into cells constitutes the infection. Once in the host’s cell, the RNA strands undergo reverse transcription in the cytoplasm and are integrated into the host’s genome, at which point the retroviral DNA is referred to as a provirus. It is difficult to detect the virus until it has infected the host, where the provirus can stay for months, even years, before becoming active and making new infectious viral particles.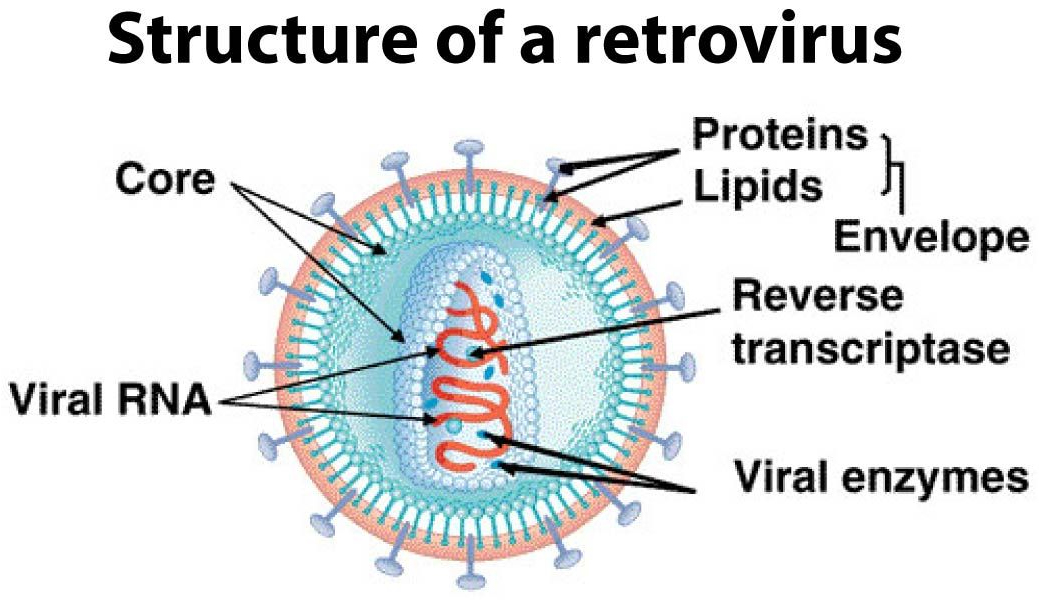
In most viruses, DNA is transcribed into RNA, and then RNA is translated into protein. Retroviruses, however, function differently. Their RNA is reverse-transcribed into DNA, which is integrated into the host cell’s genome (when it becomes a provirus), and then undergoes the usual transcription and translation processes to express the genes carried by the virus. So, the information contained in a retroviral gene is used to generate the corresponding protein via the sequence: RNA → DNA → RNA → protein. Retroviruses can be pathogens of many different hosts, including humans. A notable retrovirus is Human immunodeficiency virus (HIV), the virus responsible for acquired immunodeficiency syndrome (AIDS). As well as infecting a host, some retroviruses can cause cancer.
Retroviruses are proving to be valuable research tools in molecular biology and have been successfully used in gene delivery systems.
Besides, extensive travel is causing endemic viral species to cross borders. A unified global code of immediate reporting of new viral strains, strict surveillance and containment measures is the need of the hour.









 Latest News
Latest News General Studies
General Studies