- Home
- Prelims
- Mains
- Current Affairs
- Study Materials
- Test Series
Laws on Surrogacy and Assisted Reproductive Technology
- The Assisted Reproductive Technology (Regulation) Bill, 2020, was recently passed by Parliament.
- Live-in couples, single men, and members of the LGBTQ community are all exempt from the measure.
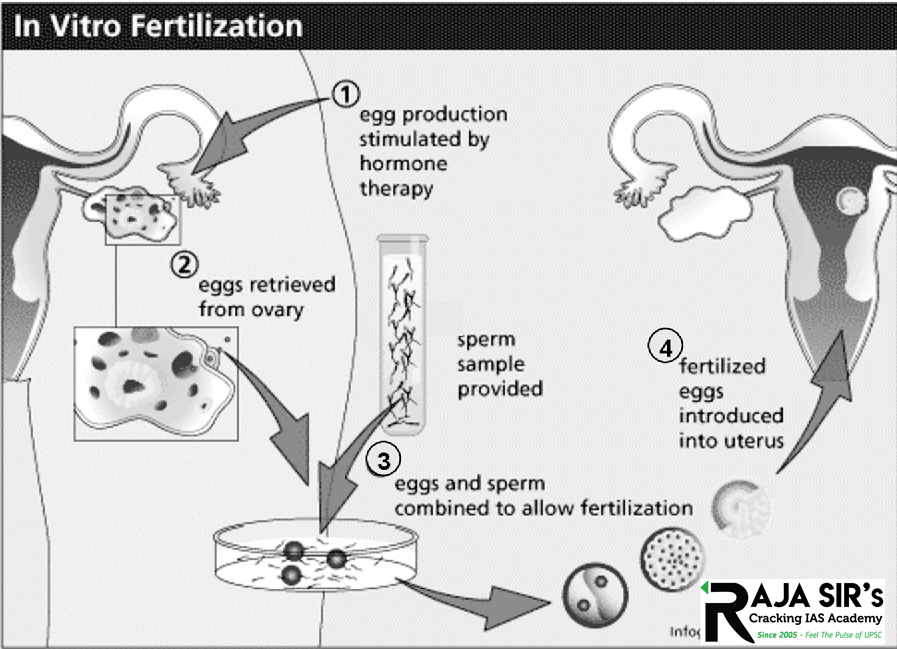
- ART is used to treat infertility.It includes fertility treatments that handle both a woman’s egg and a man’s sperm. It works by removing eggs from a woman’s body. The eggs are then mixed with sperm to make embryos. The embryos are then put back in the woman’s body.
- In Vitro fertilization (IVF)is the most common and effective type of ART.
- ART procedures sometimes use donor eggs, donor sperm, or previously frozen embryos. It may also involve a surrogate carrier.
- To Standardize Protocols: Numerous ART clinics have operated without regulation, posing a risk to the health of people who have had the process.
- India has become one of the major centers of the global fertility industry(ART), with reproductive medical tourism becoming a significant activity. This has also introduced a plethora of legal, ethical, and social issues; yet, there is no standardization of protocols and reporting is still very inadequate.
- If there is no regulation, unethical behavior will become more prevalent.
- Protection of Women and children’s rights- An insurance policy is required for the oocyte (a cell in the ovary) donor.
- The implantation of many embryos must be regulated, and children born through ART must be protected.
- The major benefit of the act would be the regulation of assisted reproductive technology services in the country. Consequently, infertile couples will be more ensured and confident of the ethical practices in ART clinics.
- A National Board that will establish a code of conduct for those who operate ART clinics.
- The Board will also establish minimum criteria for laboratory and diagnostic equipment, as well as practices that clinics and banks’ human resources must follow.
- An ART Bank is an organization that provides sperm/sperm donors, oocytes/oocyte donors, and surrogate mothers to Assisted Reproductive Technology clinics or patients.
- ART that is safe and risk-free
- The bill establishes guidelines for the safe and ethical use of assisted reproductive technologies in the country.
- The bill protects the rights of the child born through ART and ensures the confidentiality of intending spouses.
- Pre-Genetic Implantation Testing (PGIT) – required because it allows clinicians to check embryos for any faulty chromosomes before transferring them to the uterus.
- This is to prevent genetic problems in the people who are born as a result of these technologies.
- A national registry and registration authority that will keep a database to help the national Board carry out its duties.
- Punishment
- The bill proposes harsh penalties for people who engage in sex selection, sell human embryos or gametes, or run agencies/rackets/organizations that engage in such illegal activities.
- The bill stipulates that anybody implicated in the trafficking and sale of embryos will be fined Rs 10 lakh in the first instance and might be imprisoned for up to 12 years in the second case.
- Accessibility Discrimination: The Bill enables a married heterosexual couple and a woman above the age of marriage to use ARTs, but not single men, cohabiting heterosexual couples, or LGBTQ+ persons and couples.
- Redundancy: Both the Surrogacy and the ART Bills will create various registration bodies, resulting in duplication or, worse, a lack of regulation.
- Surrogacy clinics, for example, are not obligated to register surrogacy to the National
- Article 14 of India’s constitution is violated by the bill, which is also silent on children’s rights.
- Equality before the law and equal protection under the law cannot be denied to anyone in India, according to Article 14.
- Cost of Services: The procedure’s cost should be closely monitored so that even the poor can benefit from it.
- The Surrogacy (Regulation) Bill relates to surrogacy, an infertility treatment, where a third person, a woman, is the surrogate mother. In ART, treatments can be availed by the commissioning couple themselves and it is not always necessary that a third person is involved.
- Surrogacy is allowed for only Indian married couples. ART procedures are open to married couples, live-in partners, single women, and also foreigners.
- A 2015 notification prohibits the commissioning of surrogacy in India by foreigners or OCI or PIO cardholders, but NRIs holding Indian citizenship can avail of surrogacy.
- Foreigners can visit India under medical tourism to avail ART services.
- Establishment of Ethics committees – Ethics committees are required in clinics, and compulsory counseling services should be separate from them.
- Prior versions of the Bill restricted embryonic research, which must be reinstated, and definitions of “couple,” “infertility,” “ART clinics,” and “banks” must be synchronized between the Bill and the Surrogacy (Regulation) Bill.
- All ART entities shall be obligated by the national interest, cordial relations with other states, public order, decency, and morality as directed by federal and state governments.
- Before affecting millions of people, all of the constitutional, medico-legal, ethical, and regulatory concerns highlighted by the Bill must be thoroughly examined.
In-vitro Fertilization
The IVF technique was developed in the United Kingdom by Doctors Patrick Steptoe and Robert Edwards. The world's first "test-tube baby", Louise Brown, was born as a result of this technique on July 25, 1978 amid intense controversy over the safety and morality of the procedure. India's first successful IVF to produce "Durga" alias Kanupriya Agarwal-second test tube baby in the world-was performed by Dr. Subhash Mukhopadhyay on October 3, 1978. Both these events caused public debate, criticism and even social professional ostracism of those involved in initiating life outside the body. Besides these obstacles the techniques of IVF has survived as a method of choice for treating some type of infertility.
Currently, IVF success rates have improved dramatically and IVF is used by heterosexual and homosexual couples experiencing infertility as well as single women pursuing parenthood. IVF is now an established technique for treating some forms of infertility, yet it remains ethically controversial.
In-vitro Fertilization is an assisted reproductive technology (ART) commonly referred to as IVF. IVF is the process of fertilization by extracting eggs, retrieving a sperm sample and then manually combining an egg and sperm in a laboratory dish. The embryo(s) is then transferred to the uterus. Other forms of ART include gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT).
IVF Cycle- It consists- Egg Retrieval: A minor surgical procedure in which a doctor obtains eggs from the follicles of the ovaries.
- Donor Insemination: It is placed sperm directly inside the vagina at the cervix or inside the uterus (called Intrauterine Insemination or IUI). Donor insemination was previously called Artificial Insemination.
- Embryo Development: When the sperm successfully fertilizes the egg, an embryo forms and begins to grow. When the embryo is 2 to 3 days old it at the ‘cleavage stage’; at 5 to 6 days old, it is called a ‘blastocyst’.
- Embryo Transfer: Fertilized eggs (embryos) are placed back into the woman’s uterus or fallopian tube through the cervix.
 Treat Different Types of Infertility
Treat Different Types of Infertility
- IVF can be used to Treat Infertility of Different Types such as-
- Blocked or damaged fallopian tubes.
- Male factor infertility including decreased sperm count or sperm motility.
- Women with ovulation disorders, premature ovarian failure and uterine fibroids.
- Women who have had their fallopian tubes removed.
- Individuals with a genetic disorder.
- Unexplained infertility.
| In-vivo fertilization | In-vitro fertilization |
| In-vivo fertilization refers to the normal method of fertilization between female egg and male sperm within a human body. | In-vitro fertilization refers to the artificial method of fertilization between female egg and male sperm outside a human body. |
| The term in-vivo came from the Latin word “within the living”. | The term in-vitro came from the Latin word “within the glass”. |
| It is a natural/normal method of reproduction that occurs in uterus/womb of female body. | It is an artificial method of reproduction done in laboratory using different humanized techniques. |
| This method of fertilization is normal and natural among couples. | This method of fertilization is chosen to cure infertility in human, either male or female. |
| It is a non-surgical method of fertilization. | It is a surgical method of fertilization. |
| Babies born through this method are considered as normal babies. | Babies born through this method are called ‘test-tube-baby’. |
| From chemical perspective, during in-vivo fertilization all chemical reactions between the egg and sperm occur within the human body. | From chemical perspective, during in-vitro fertilization all chemical reactions between egg and sperm is conducted in laboratory. |
| None of the chemical changes and reactions are in human control as everything occurs within human body. | All the chemical changes and reactions are in human control/in a controlled environment as this fertilization is conducted outside human body. |
| It is a simpler technique of fertilization. | It is relatively a more complex technique as it involves surgical procedure to retrieve the eggs. |
| The cost per treatment is lower. | Cost per treatment is higher and causes higher financial burden. |
| This method provides limited information during check up and treatment. | This method provides valuable information during treatment as the reactions between egg and sperms are evaluated initially in the lab setting. |
| It can be also considered as an experiment done using a whole living organism. | It can be also considered as an experiment done outside living organism. |
| This method of fertilization is suitable for fertile couple who don’t have any reproductive health complications. | This method of fertilization is suitable for infertile couple/s that has some complication related to reproductive organs. |
| It is a not an assisted method of fertilization. | It is a physician assisted method of fertilization. |
| This method does not have risk of multiple pregnancy. | The risk associated with this method is the possibility of multiple pregnancy. |
- IVF increases the risk of multiple births if more than one embryo is implanted in the uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.
- Use of IVF slightly increases the risk that a baby will be born early or with a low birth weight.
- Use of injectable fertility drugs can cause OHS, in which ovaries become swollen and painful.
- The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15 to 25 percent — but the rate increases with maternal age.
- The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived.
The reproductive revolution has had the ability to separate genetic parenting from gestational parenting and from social parenting and the agent who brings it all about, a biotechnical, will be still another person. Sperm and eggs are being brought and sold and wombs are being rented. The fact, that these techniques have been developed and have a certain success rate does not make them morally acceptable.
Donation of sperms and ova are both contrary to the unity of marriage and the dignity of procreation of human being. Furthermore, these procedures lend themselves to commercialization and exploitation, when people are being paid for sperm, ova and for surrogate motherhood.
Some of the ethical issues involved in this technology are:- Bypassing the natural method of conception.
- Creating life in laboratory.
- Fertilizing more embryos than will be needed.
- Discarding excess embryos.
- Expensive technology, not affordable for common man.
- Creating embryos, freezing them and keeping them in limbo.
- Destroying embryos in research.
- Selective termination of embryos etc.
The legal problems that arise from invitro fertilization are that number of persons can assert for parental rights extends to the sperm donor, the egg donor, the surrogate mother, parents who raise the child. Further, if during the time in which the embryos are in storage, the couple divorces, legal complications may arise as to the custody of the embryo. The spare embryos are frozen, discarded, donated or used for experimentation. Since some religions believe that life begins at conception, it may amount to abortion which is contrary to both law and ethics. Expert indentation is also not permissible as science cannot experiment with someone with basic human rights without prior permission. Donation involves separation of the biological and social roles of parenthood that is significant part of family concept and is equivalent to adoption before birth thereby calling for amendments in adoption laws of most of the countries. When she is carrying more developed embryos, it can endanger her life. The only alternative available to avoid risk to her health and life is to carry out selective termination of one or more of the developing embryos. This not only involves trading of one life or more but the doctor is faced with the decision of which ones to terminate and how to make this decision.
The Indian Council for Medical Research (ICMR) Guidelines It is necessary to follow ICMR guidelines in ascertain the therapeutic and research values of the Assistive Reproductive (AR) procedure. Informed Consent After duly counselling the couple/ oocyte/semen donor, an informed and written consent should be taken from both the spouses as well as the donor. Selection of Donor The semen bank assumes the responsibility in selection of the suitable donor on following terms:- The physical characteristic and mental make-up of the donor should match as closely as possible to that of the spouse of the recipient, especially with reference to colour, eyes and hair, height and build, religious and ethnic background, and education and ABO blood type.
- Blood group of the proposed donor and donee should be tested with respect to Rh compatibility.
- No donor suffering from any sexually transmitted disease (e.g. syphilis, gonorrhea, chlamydia, herpes, HIV etc.), infectious disease (e.g. hepatitis B and C, HIV) or genetically transmissible disease. Sexually transmitted diseases should be ruled out within a week of obtaining the seminal fluid.
- It is essential that donated semen is cryo-preserved and used only after 6 months as this would enable the centre to retest the donor after 6 months for HIV and eliminate the potential risk of HIV transmission in the ‘window’ period of HIV infection.
- Identity of the donor as well as the recipient should be protected from each other. However, all the records of the donor must be preserved for at least 10 years and should be confidential.
- Confidentiality of the entire procedure and its outcome is advisable and therefore, no relative should be accepted as a donor in order to avoid identification and claims of parenthood and inheritance rights.
- Any information about clients and donors must be kept confidential. No information about the treatment of couples may be disclosed to anyone other than the accreditation authority or persons covered by the license, except with the consent of the person(s) to whom the information relates, or in a medical emergency concerning the patient, or a court order.
- Written consent and an undertaking of the donor should be taken towards unrestricted use of sperms or oocytes for AR and he/she will not attempt to seek the identity of the recipient.
IVF has emerged as one of the most widely adopted and successful medical technologies in the last century. While giving hope to millions of couples suffering from infertility, IVF also has presented new ethical, legal, and social questions that society must address. Many countries have taken steps to regulate certain aspects of IVF. Specifically, what regulations and laws should be in place for IVF reporting, social inequities that may arise from financial barriers to IVF, genetic testing, emerging laboratory techniques that have improved embryo and gamete survival when cryopreserved and an individual’s right to their genetic offspring in the setting of gamete or embryo donation are aspects of IVF which will become increasingly controversial and debated into the future.
However, the lion’s share of ethical and legal questions that exist surrounding IVF have yet to be resolved. Society must reconcile how to fund IVF in a responsible and equitable manner to increase access to care. Additionally, the myriad of unresolved issues surrounding gamete and embryo donation must be addressed in greater detail in future social and legal dialogues.









 Latest News
Latest News
 General Studies
General Studies