- Home
- Prelims
- Mains
- Current Affairs
- Study Materials
- Test Series
AMR- PPP 100 - PRELIMS 2024 - 13
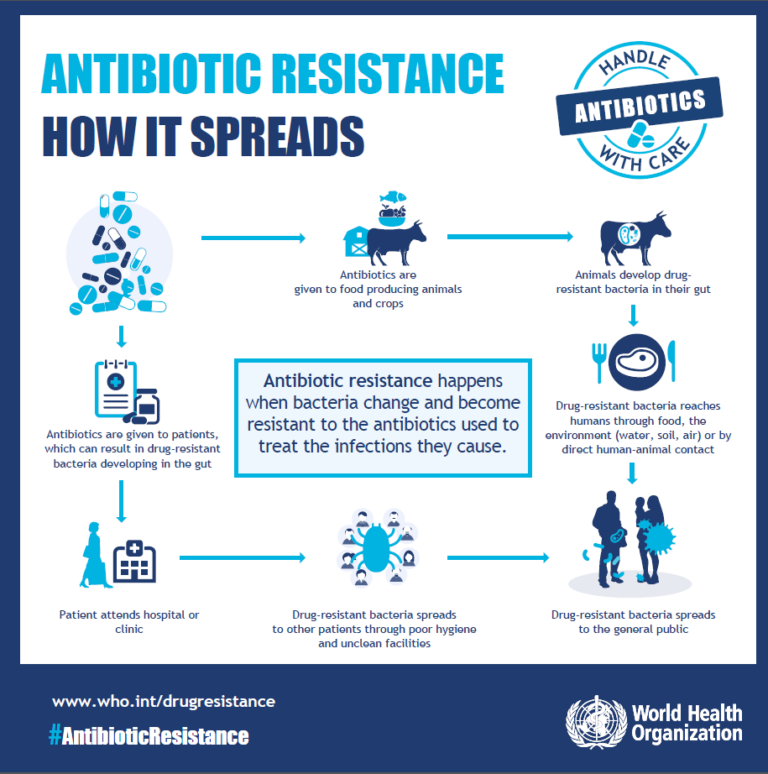
Antimicrobial resistance occurs when microbes (bacteria, viruses, fungi and parasites) become resistant to antimicrobial drugs (such as antibiotics, anti-fungals, antivirals, antimalarials, and anthelmintics).As a result, the medicines become ineffective and infections persist in the body, increasing the risk of spread to others.India has witnessed an increase in antibiotic consumption- about 65 per cent in 2015 compared to 2000, while the rate of consumption increased from 3.2 to 6.5 billion daily defined doses (DDDs) in the same period. Recently, government has banned colistin- a last line of antibiotic in the poultry industry due to rise in cases of antibiotic resistance against it.
Various Causes of antibiotic resistance: Microbes can become resistant to drugs for both biological and social reasons.
- Microbial behaviour:As soon as scientists introduce a new antimicrobial drug, there is a good chance that it will become ineffective at some point in time. This is due primarily to changes occurring within the microbes.
- People’s behaviour:Not following recommendations for the use of some drugs can increase the risk of antimicrobial resistance. The way in which people use antimicrobial drugs is a significant contributing factor. Some individualistic reasons are:
- Wrong diagnosis: Doctors sometimes prescribe antimicrobials “just in case,” or they prescribe broad-spectrum antimicrobials when a specific drug would be more suitable. Using these medications in this way increases the risk of AMR.
- Inappropriate use: If a person does not complete a course of antimicrobial drugs, some microbes may survive and develop resistance to the drug. Also antibiotics recommended by quacks or pharmacist contribute to magnify the issue.
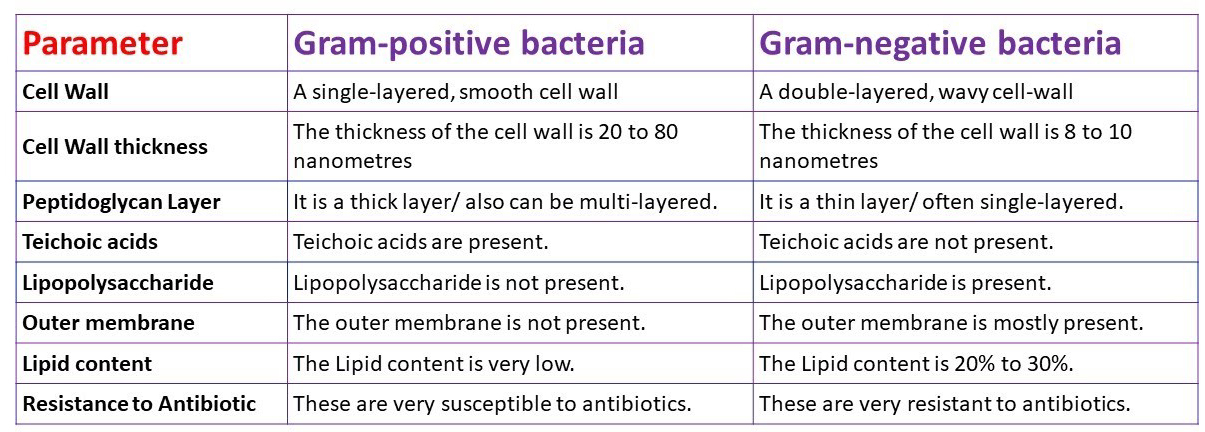
- Agricultural use:Using antibiotics in farm animals can promote drug resistance. Scientists have found drug-resistant bacteria in meat and food crops that have exposure to fertilisers or contaminated water. In this way, diseases that affect animals can pass to humans.
- Hospital use: People who are critically ill often receive high doses of antimicrobials. This encourages the spread of AMR microbes, particularly in an environment where various diseases are present.

|
Acinetobacter baumannii The U.S. Food and Drug Administration has approved Xacduro as a new treatment for hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia caused by Acinetobacter baumannii-calcoaceticus complex (A. baumannii).
“Red alert” pathogen”
Locomotion
Impact
Habitat
|
Government initiative against AMR:
- India’s National Action Plan (NAP) for AMR was released in 2017 by the Union Ministry of Health and Family Welfare. The objectives of the NAP include:
- Improving awareness and enhancing surveillance measures.
- Strengthening infection prevention and control.
- Research and development, promoting investments, and collaborative activities to control AMR.
On the basis of the NAP, various states have begun the process of initiating their State Action Plans. The challenges in implementation of NAP are as varied perceptions about antibiotic use and AMR among key stakeholders, lack of diagnostic facilities, widespread use of antibiotics in various sectors, environmental contamination because of pharmaceutical industry, etc. Thus, inter-sectoral co-ordination between public and private sectors and comprehensive strengthening of the healthcare systems are necessary to achieve the desired forward momentum.
- Muscat Manifesto - At the Third Global High-Level Ministerial Conference on Antimicrobial Resistance held in Muscat, over 30 countries adopted the Muscat Ministerial Manifesto on AMR.The Muscat Manifesto recognised the need to accelerate political commitments in the implementation of One Health Action for controlling the spread of AMR. The conference focused on three health targets
- Reduce the total amount of antimicrobials used in the agri-food system at least by 30-50% by 2030
- Eliminate use in animals and food production of antimicrobials that are medically important for human health
- Ensure that by 2030 at least 60% of overall antibiotic consumption in humans is from the WHO “Access” group of antibiotics
- Reporting to GLASS- India plans to strengthen private sector engagement and the reporting of data to the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS).
- The National Health Policy 2017– It has offered specific guidelines regarding use and limiting the use of antibiotics as over-the-counter medications and restricting their usage in livestock. It also called for scrutiny of prescriptions to assess antibiotic usage in hospitals and among doctors.
- Signing the Delhi Declaration on AMR:The Delhi Declaration on Antimicrobial Resistance (AMR) is an inter-ministerial consensus that was signed by the ministers of the concerned ministries in India.
- The declaration aims to address AMR in a mission mode by involving research institutes, civil society, industry, small- and medium-sized enterprises, and encouraging public-private partnerships.
- Antibiotic Stewardship Program (AMSP): The Indian Council of Medical Research (ICMR) has initiated the AMSP on a pilot project basis in 20 tertiary care hospitals across India. The program aims to control the misuse and overuse of antibiotics in hospital wards and ICUs.
- Ban on inappropriate fixed dose combinations (FDCs): On the recommendations of the ICMR, the Drug Controller General of India (DCGI) has banned 40 FDCs that were found to be inappropriate.
- Ban on the use of Colistin as a growth promoter in animal feed:The ICMR, in collaboration with the Indian Council of Agriculture Research, Department of Animal Husbandry, Dairy and Fisheries, and the DCGI, has banned the use of Colistin as a growth promoter in animal feed in poultry.
- One Health approach:The government is working on a One Health approach by encouraging interdisciplinary collaboration at the human-animal-environmental interface. The key priority areas include zoonotic diseases, food safety, and antibiotic resistance.
- Integrated One Health Surveillance Network for AMR: The ICMR has undertaken a project on an "Integrated One Health Surveillance Network for Antimicrobial Resistance" in collaboration with the Indian Council of Agriculture Research to assess the preparedness of Indian Veterinary laboratories to participate in an integrated AMR surveillance network.
|
Medicines Patent Pool Agreement for Leukaemia Recently, the Medicines Patent Pool (MPP), a United Nations-backed group signed sub-licence agreements with three India-based companies to make certain Cancer Drugs more accessible and cheaper for patients. § These agreements allow the production of generic versions of Novartis'' cancer treatment drug Nilotinib, primarily used for Chronic Myeloid Leukaemia (CML), in several countries. § The licence covers India, seven middle-income countries, and 44 territories, allowing the generic versions of Nilotinib to be supplied, subject to local regulatory authorization. Medicines Patent Pool § MPP is a United Nations-backed public health organisation working to increase access to, and facilitate the development of, life-saving medicines for Low- and Middle-Income Countries (LMIC). § It was founded in July 2010, based in Geneva, Switzerland. § MPP partners with civil society, governments, international organisations, industry, patient groups, and other stakeholders, to prioritise and license needed medicines and pool Intellectual Property to encourage generic manufacture and the development of new formulations. § As of now, MPP has signed agreements with twelve patent holders for thirteen Human Immunodeficiency Virus (HIV) antiretrovirals, one HIV technology platform, three hepatitis C direct-acting antivirals, a tuberculosis treatment, a long-acting technology, two experimental oral antiviral treatments for Covid-19 and a Covid-19 serological antibody technology. Chronic Myeloid Leukaemia (CML) o It is one of the types of Leukemia, which is a blood-cell cancer that affects the bone marrow and the blood. Other types are, · Acute Lymphoblastic Leukemia (ALL) · Acute Myeloid Leukemia (AML) · Chronic Lymphocytic Leukemia (CLL). o It is characterized by the uncontrolled growth of abnormal white blood cells called myeloid cells. o CML typically progresses slowly, and it is often diagnosed during the chronic phase. § Diagnosis: o CML is typically diagnosed through a combination of blood tests and bone marrow examination. |
Prevention and control measures:
- Individuals:To prevent and control the spread of antibiotic resistance, individuals should:
- Only use antibiotics when prescribed by a certified health professional.
- Never demand antibiotics if your health worker says you don’t need them.
- Always follow your health worker’s advice when using antibiotics.
- Never share or use leftover antibiotics.
- Policy makers: To prevent and control the spread of antibiotic resistance, policy makers should:
- Ensure a robust national action plan to tackle antibiotic resistance is in place.
- Improve surveillance of antibiotic-resistant infections.
- Strengthen policies, programmes, and implementation of infection prevention and control measures.
- Regulate and promote the appropriate use and disposal of quality medicines.
- Make information available on the impact of antibiotic resistance.
- Health professionals:To prevent and control the spread of antibiotic resistance, health professionals should:
- Prevent infections by ensuring that their hands, instruments, and environment are clean.
- Only prescribe antibiotics when they are needed, according to current guidelines.
- Report antibiotic-resistant infections to surveillance teams.
- Agriculture sector:To prevent and control the spread of antibiotic resistance, the agriculture sector should:
- Only give antibiotics to animals under veterinary supervision.
- Not use antibiotics for growth promotion or to prevent diseases in healthy animals.
- Vaccinate animals to reduce the need for antibiotics and use alternatives to antibiotics when available.
- Promote and apply good practices at all steps of production and processing of foods from animal and plant sources.
- Improve biosecurity on farms and prevent infections through improved hygiene and animal welfare.
There is need to urgently address antimicrobial resistance through the lens of one (human, animal and environment) health. All countries need to work together to limit the spread of ARGs and antibiotics between humans, animals and the environment in the globalised world where we live. Even though national action plans have been laid down by most countries, these plans have yet to move from paper to the ground as antibiotics continue to be freely used.
PYQ
Which of the following are the reasons for the occurrence of multi-drug resistance in microbial pathogens in India? (2019)
1. Genetic predisposition of some people
2. Taking incorrect doses of antibiotics to cure diseases
3. Using antibiotics in livestock farming
4. Multiple chronic diseases in some people
Select the correct answer using the code given below.
(a) 1 and 2
(b) 2 and 3 only
(c) 1, 3 and 4
(d) 2, 3 and 4









 Latest News
Latest News
 General Studies
General Studies