- Home
- Prelims
- Mains
- Current Affairs
- Study Materials
- Test Series
Drug-resistant typhoid strains
Bacteria that cause typhoid fever are becoming more and more resistant to some of the most widely used antibiotics, according to the study published in The Lancet Microbe journal.
-
Typhoid fever causes 11 million infections and more than 1,00,000 deaths per year. South Asia accounts for 70% of the global disease burden.
Typhoid
-
-
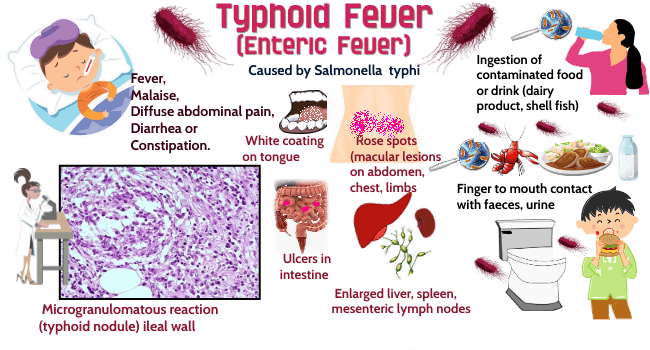
Typhoid fever is a life-threatening systemic infection caused by the bacterium Salmonella enterica serovar Typhi (commonly known as Salmonella Typhi) carried only by humans – no other animal carrier has been found.
-
-
Transmission:
-
Typhoid fever is transmitted by the faecal-oral route, through ingestion of contaminated food or water.
-
Without treatment, about one person in 20 who recovers from typhoid becomes a ‘carrier’. Despite having no symptoms of illness, they have bacteria in their faeces and urine, and can infect others for a period of about three months (sometimes up to one year).
-
Travellers are at high risk of developing typhoid fever in many typhoid endemic countries. This includes parts of Asia (especially India, Pakistan, and Bangladesh), Africa, the Caribbean, Central and South America, and the Middle East.
-
-
Symptoms:
-
Symptoms and signs of typhoid range from mild to severe, can last for about one month without treatment, and may include: fever, fatigue or tiredness, malaise (general feeling of unwellness), sore throat, persistent cough, headache.
-
-
Prevention:
-
Vaccine:
-
The typhoid vaccine is available as an oral medication or a one-off injection:
-
Capsule: For adults and children over the age of 6 years, this is a live, attenuated vaccine.
-
Shot: For adults and children over the age of 2 years, this is an inactivated vaccine a person needs to get 2 weeks before travel.
-
The typhoid vaccine is only 50–80% effective.
-
-
-
-
Treatment:
-
Typhoid fever requires prompt treatment with antibiotics.
-
-
Drug Resistance:
-
The effectiveness of antibiotics for typhoid fever is threatened by the emergence of drug resistant strains.
-
The existence of resistant strains of bacteria means antibiotics or drugs designed to kill them no longer work, allowing them to spread rapidly, posing a risk to public health.
-
-
Since 2000, multi-drug-resistant (MDR) typhoid has declined steadily in Bangladesh and India, remained low in Nepal, and increased slightly in Pakistan.
-
However, these are being replaced by strains resistant to other antibiotics, according to the study conducted by researchers from Stanford University, Christian Medical College Vellore and other institutions.
-
Multi-drug resistance (MDR) is defined as lack of susceptibility to at least one agent in three or more chemical classes of antibiotic.
-
Strains were classified as MDR if they had genes giving resistance to antibiotics ampicillin, chloramphenicol, and trimethoprim/ sulfamethoxazole.
-
-
A new type of drug resistance is observed in strains termed XDR typhoid. Strains resistant to the antibiotic (azithromycin) have been seen in India, Bangladesh, Nepal and Pakistan.
-
Extensive Drug Resistance (XDR) typhoid is caused by a strain that is resistant to at least five antibiotic classes recommended for treating typhoid fever.
-
-
Road ahead
-
An integrative approach and a comprehensive policy framework are required to be in place for the prevention, control and elimination of typhoid fever.
-
India’s Health Ministry is considering introducing new typhoid conjugate vaccines into the national immunization program. Two WHO prequalified vaccines have been developed in India (by Bharat Biotech and Biological E).









 Latest News
Latest News
 General Studies
General Studies